SIERRA LEONE
Just under half of Sierra Leone’s urban population is projected to live in the capital, Freetown by the year 2028. During the civil war of 1992-2002, the capital experienced a high influx of internally displaced people from the provinces. Coupled with natural population growth and the continued shift from rural areas to the cities, the proliferation of informal settlements and a recovering health system, poses a major health challenge.
Health and social issues
In Freetown, most of the official health statistics and surveys do not adequately capture the range of health problems experienced by poor people living in informal urban settlements. The lack of disaggregated data on different informal communities indicates that appropriate policies may not be in place. No known study has been conducted to bring together perspectives on the range of problems, contexts and approaches.
Many informal urban settlement dwellers face a variety of risks related to their environment, including those associated with natural disasters (e.g. flooding), overcrowding, poor housing, poor waste disposal systems and air pollution (including the burning of waste), poor sanitation and inadequate water supply. These fuel the rapid spread of communicable diseases. The health system’s capacity for disease control is poor. Poor and marginalised communities are affected more severely by these health hazards. Poor nutrition, high rates of maternal mortality, teen pregnancies and sexually transmitted infections (STIs) disproportionately affect poor households living in informal settlements. The burden of disability is high. Largely as a result of poor drainage, flooding has become nearly an annual event in Freetown in the last four years, leading to the collapse of houses, loss of property, deaths, injuries, destruction of toilets and contamination of water sources. Because data are limited on the scale of risks faced by informal urban settlement dwellers, the Government of Sierra Leone and NGOs have struggled to plan and coordinate effective responses to improve health.
Studies identify a range of barriers faced by people in informal settlements in accessing formal health care, including costs (direct and indirect), limited geographic accessibility, socio-cultural obstacles, distance, long waiting times and limited availability of services.
Governance
Despite efforts to build effective, inclusive and accountable governance in the post-conflict era, the recent Ebola epidemic illustrated the weakness of the health system as well as lack of trust between citizens and the state. Most people have to pay for services from a mix of public and private suppliers. The country faces considerable challenges in training and retaining health workers. . The City of Freetown elected a new mayor in March 2018. Yvonne Aki Sawyerr (Freetown’s first female mayor in 35 years) was an active responder to the Ebola crisis and seeks to transform Freetown’s health sector and is committed to working with the Federation of the Urban and Rural Poor (SDI’s affiliate in Sierra Leone) to undertake this work in informal settlements where health outcomes are at their weakest.
SLURC conducted a review of government policies from the perspective of informal settlements. They found that because the health sector has been slow to realise the particular problems posed by rapid urbanisation to health care delivery in urban areas, the health policy framework is general, with no specific reference to urban health. Policies not only ignore informal communities’ specific health problems and needs, but also their role in health care delivery. Only a few policies, such as the new community health worker policy developed in 2016, are open to community inclusion in health care delivery. A number of policies do not refer to environmental health, including the potential for communities and their groups to work with the government (central and municipal) to mitigate environmental health risks. It is not clear to what extent people living in informal settlements are aware of relevant policies. This knowledge could, however, enable them to hold health organisations accountable, and shape interventions to meet community needs.
The Federation of the Urban and Rural Poor – Sierra Leone, organizes slum communities in five cities and has approximately 10,300 members. Key priorities for the Sierra Leone federation include improving community and household capacity to mitigate and bounce back from disasters and shocks; increase federation membership, saving and livelihood opportunities for the urban poor; and ensure the urban poor are active partners in the development and implementation of the Freetown city development plan and government’s New Direction national development plan. Following city wide profiling, the federation is eager to ensure its information informs action. Indeed, the federation has undertaken many small upgrading projects to improve accessibility in slums, to improve access to basic services such as toilets and waste management, retaining walls and to develop settlement upgrading plans. Under the slogan, “my data, my knowledge, my action” the alliance aims to show government how to operationalize a new direction and produce more inclusive development and ensure slum upgrading is recognized as a central strategy for building urban resilience, disaster risk management, and climate change adaptation.
A stakeholder workshop identified over 13 organisations that are currently active in informal settlements. Apart from the Ministry of Health and Sanitation and its key agencies, nearly all the other actors — mostly NGOs and a few community-based organisations (CBOs) — operate at the subnational level. These organisations’ responses are uncoordinated and duplicated, and rarely informed by evidence. This creates a window of opportunity for the ARISE project to support coordination activities and research into action. Most health interventions focus on cholera and diarrhoea, nutrition and child health and wellbeing, the promotion of safer sex and treatment of STIs. Few interventions deal with environmental health threats, health education, mental health and occupation-related health problems at the community level.
Read more
Annie Wilkinson & James Fairhead (2017) Comparison of social resistance to Ebola response in Sierra Leone and Guinea suggests explanations lie in political configurations not culture, Critical Public Health, 27:1, 14-27
SDI Know your city website
Posts on Sierra-leone
WASH-related violence in urban informal settlements in Bangladesh, Kenya, India and Sierra Leone: Co-producing knowledge for just health systems
A poster, presented at Bintu Mansaray, Rosie Steege, Samira Sesay, Inviolata Njeri Njoroge, Ivy Chumo, Caroline Kabaria, Blessing Mberu, Partho Mukherjee, Surekha Garimella, Riaz Hossain, Sabina Rashid, Rachel Tolhurst, Neele Wiltgen Georgi, Kate Hawkins, Sally Theobald and Laura Dean, at the 8th Global Symposium on Health Systems Research. Urban informal settlements are characterised by poor […]

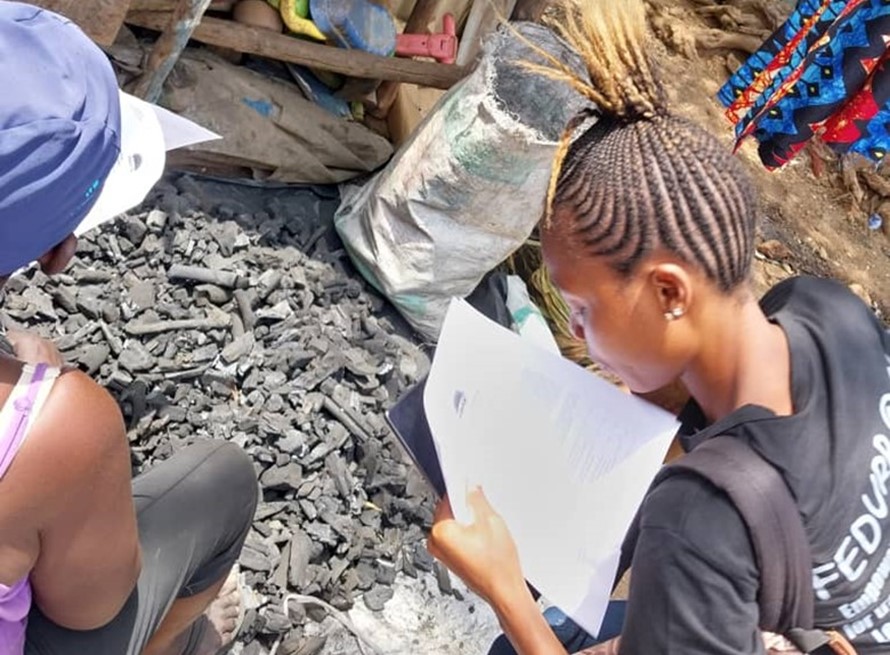
Impact Case Study: Community researchers’ roles in achieving ARISE outcomes and legacy
ARISE aimed to explore and understand the health and well-being of people and communities working and living in informal spaces, which can be influenced by a combination of factors such as residence, environmental conditions, financial status, educational attainment and social connections with friends and family. There is evidence that the close involvement of co-researchers at […]
Impact Case Study: Community sensitive emergency measures taken during COVID-19 in informal settlements in Freetown, Sierra Leone
The participatory and inclusive approach employed by the ARISE Sierra Leone partners strengthened relationships and trust between communities and the government agency responsible for the COVID-19 response at the district level (DICOVERC – District COVID-19 Emergency Response Centre). This created a more open and conducive environment for health service uptake within these communities. ARISE created […]
Health and wellbeing survey of informal settlements in Freetown, Sierra Leone, May 2023
In May 2023 a health and wellbeing survey of informal settlement residents in Cockle Bay, Moyiba and Dwazark, in Freetown, Sierra Leone was undertaken by ARISE partners. This blog acts as a summary, highlighting some of the main findings. We also have the full survey report available for download. Background This survey builds on the […]